
What is Gastroparesis?
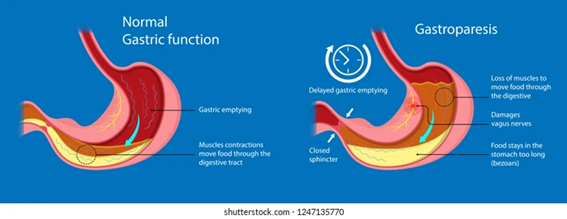
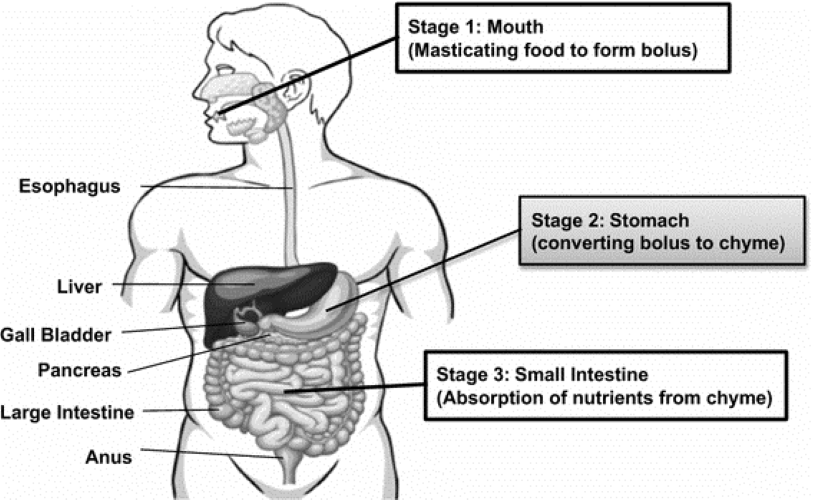
Gastroparesis is defined by delayed gastric emptying without any mechanical obstruction. This condition results in the stomach taking an extended time to empty its contents into the small intestine, leading to symptoms such as nausea, vomiting, abdominal pain, bloating, and early satiety. The precise cause of gastroparesis is frequently unknown, but it can be associated with diabetes, surgeries, infections, and certain medications. (Sullivan, Temperley, & Ruban, 2020).
Key Facts from Research:
According to the Cleveland Clinic (Araujo-Duran, Chatterjee, & Garg, 2024), gastroparesis affects an estimated 1.5 to 5 million Americans, predominantly women. This condition occurs when the stomach muscles or the nerves controlling them are damaged, leading to delayed gastric emptying. Key points from the article include:
- Symptoms: Patients often experience nausea, vomiting, bloating, and an early “full” feeling due to slow digestion (Araujo-Duran et al., 2024).
- Causes: Damage to the nerves that activate your stomach muscles is the main cause of gastroparesis. The overall result is that the muscle contractions that churn food in your stomach and then squeeze it out through the bottom are impaired. This leads to indigestion and delayed gastric emptying — food sitting too long in your stomach. Around one-third of people with diabetes (Type 1 or Type 2) develop gastroparesis. It happens when high blood sugar levels damage your nerves. High blood sugar levels also damage the blood vessels that carry oxygen to your tissues, so your stomach nerves and muscles are both affected. Other less common causes can include surgery, infection, autoimmune disease, and some medications (Araujo-Duran et al., 2024).
- Complications: Chronic nausea and vomiting, or simply the loss of appetite, can lead to weight loss and malnutrition. Gastroparesis can increase acid reflux, and chronic acid reflux may cause esophageal complications. Gastroparesis can also affect blood sugar. When food sits for too long in your stomach, your blood sugar may drop too low. When food finally releases, your blood sugar may spike (Araujo-Duran et al., 2024).
- Diagnosis: Tests such as gastric emptying studies, gastric motility tests, and imaging help diagnose gastroparesis (Araujo-Duran et al., 2024).
- Treatment: Healthcare providers can’t directly fix the damage that causes gastroparesis, but they can offer treatment to stimulate muscle contractions in your stomach and encourage it to empty. Medication is the first treatment method; if it doesn’t help, then surgery may be an option. Management focuses on dietary changes, keeping up with medications, and following any post-surgery instructions (Araujo-Duran et al., 2024).
Get Involved
During Digestive Tract Paralysis Awareness Month, it’s crucial to spread knowledge about gastroparesis and support those living with this condition. Here are some ways you can get involved:
- Educate Yourself and Others: Learn about the symptoms, causes, and treatments of gastroparesis. Share this information with your community to help others recognize the signs and seek appropriate care.
- Support Research and Advocacy: Contribute to organizations that fund research on gastroparesis and advocate for better patient care. Your support can help drive advancements in understanding and treating this condition.
- Participate in Awareness Campaigns: Join social media campaigns, attend events, and use hashtags like #LivingWithGP to share your story and connect with others affected by gastroparesis.
By raising awareness and supporting research, we can improve the lives of those living with gastroparesis and work towards better treatments and ultimately, a cure.
References:
- Araujo-Duran, J., Chatterjee, A., & Garg, S. (2024). Gastroparesis for the nongastroenterologist. Cleveland Clinic Journal of Medicine, 91(6), 373-383. https://doi.org/10.3949/ccjm.91a.23078
- Sullivan, A., Temperley, L., & Ruban, A. (2020). Pathophysiology, aetiology and treatment of gastroparesis. Digestive Diseases and Sciences, 65(6), 1615-1631. https://doi.org/10.1007/s10620-020-06287-2
Fullscript Products:
At Integrated Holistic Solutions PLLC,we have a variety of wellness products to support patients diagnosed with gastroparesis that are available at https://integratedholisticsolutions.com/fullscript/ Some items that may be helpful for individuals with gastroparesis include:

These statements have not been evaluated by the Food and Drug Administration. These products are meant for general use only and are not intended to diagnose, cure, treat, or prevent any disease. Any decision to use supplements to support your specific needs should be considered in partnership with your licensed healthcare practitioner.
